Feeling Unheard at the Doctor? Here's How to Change That.
In this blog, I interchange the words patient and service user and refer to a clinician as a service provider- anyone that provides healthcare services, including physicians, surgeons, nurses, midwives, technicians, therapists, etc.
I’ll never forget sitting with a patient in my Edinburgh clinic, her eyes brimming with tears as she described feeling dismissed during a previous appointment about her heavy, painful periods.
- she’d waited 9 years to be diagnosed with endometriosis, a common condition that affects 1 in 10 women.
Not being heard. Not being told. Not enough time.
Have you ever left a doctor’s visit feeling like your concerns were brushed aside? Maybe you mentioned pelvic pain, only to be told it’s “normal,” or felt overwhelmed by medical terms without clear answers? You’re not alone.
Evidence suggests that clinicians interrupt patients within 20 seconds of speaking and only spend 5% of the conversation answering questions.
It’s not uncommon for patients to leave clinics with either too little or too much information & jargon. Clinicians also report feeling frustrated about not meeting patients' needs.
This blog equips you—whether a patient or clinician—with tools to make shared decision-making a reality, particularly in women’s health.
To do this, I’d like you to imagine 2 things:
The patient and clinician are on the same team.
There are always two experts in the consultation room- you are one of them.
Shared Decision-Making: What Matters To You?
Shared decision-making (SDM) is about teamwork—you and your clinician deciding together what’s best for you. It’s not me dictating a treatment plan; it’s us talking through your options, like whether surgery or watchful waiting suits your fibroid symptoms, or what birth plan feels right for you. The 2022 Realistic Medicine report calls this personalised care, and I’ve seen it work wonders in my practice. When I ask, “What matters to you? or “What’s keeping you up at night?” or” What do you think might be going on?”—maybe over a cup of tea in my mind’s eye—I hear what’s really on your heart, and we get to the core of your needs faster.
SDM takes time, sure, but it also saves time. By focusing on what matters to you, we avoid going down rabbit holes of irrelevant tests or treatments. For example, one patient told me her biggest worry was balancing menopause treatment with her demanding job. Once I knew that, we crafted a plan that fit her life, no extra appointments needed.
Shared Decision Making Takes Culture & Power into Context
Translating ‘ what do you think is going on?’ Could be -What’s keeping you up at night? What are you scared to tell your partner about? What have heard about ‘x’ from your friends(or the internet)?
What If the Response is ‘ You’re the Expert-You Tell Me’
I’ve had attempts at SDM slap me in the face. My fondest memory of this was when I attempted my routine approach with an African Auntie. Her response- ‘Didn’t you go to medical school? You should be the one telling me.’
Acknowledging the cultural contexts of roles and power dynamics between care providers and users is critical. As clinicians, verbally acknowledging how important a patient’s perspective is in their care plan can be empowering. It gives people permission to share, contradict and question.
To ensure that you make the most of your upcoming appointment with your gynaecologist or any other healthcare professional, it is crucial to communicate your concerns and priorities to your medical team effectively. What matters to you?
Remember, providers exist for patients, not the other way round.
There Are Always (at least) Two Experts in the Room
Whilst as a patient you cannot compare your Google search to my 2+ decades of experience, as a clinician I cannot compare my medical education to your 2+ decades of living with that condition.
Despite decades of medical education and specialist training, no clinician will ever know your body more than you will. As a patient, this is your lived expertise. Both lived experience and professional expertise are important in shared decision-making.
If you’re dealing with endometriosis, heavy periods, navigating fertility challenges or perimenopause symptoms, lean into your lived experience. Your insights are gold and shape the shared decision-making.
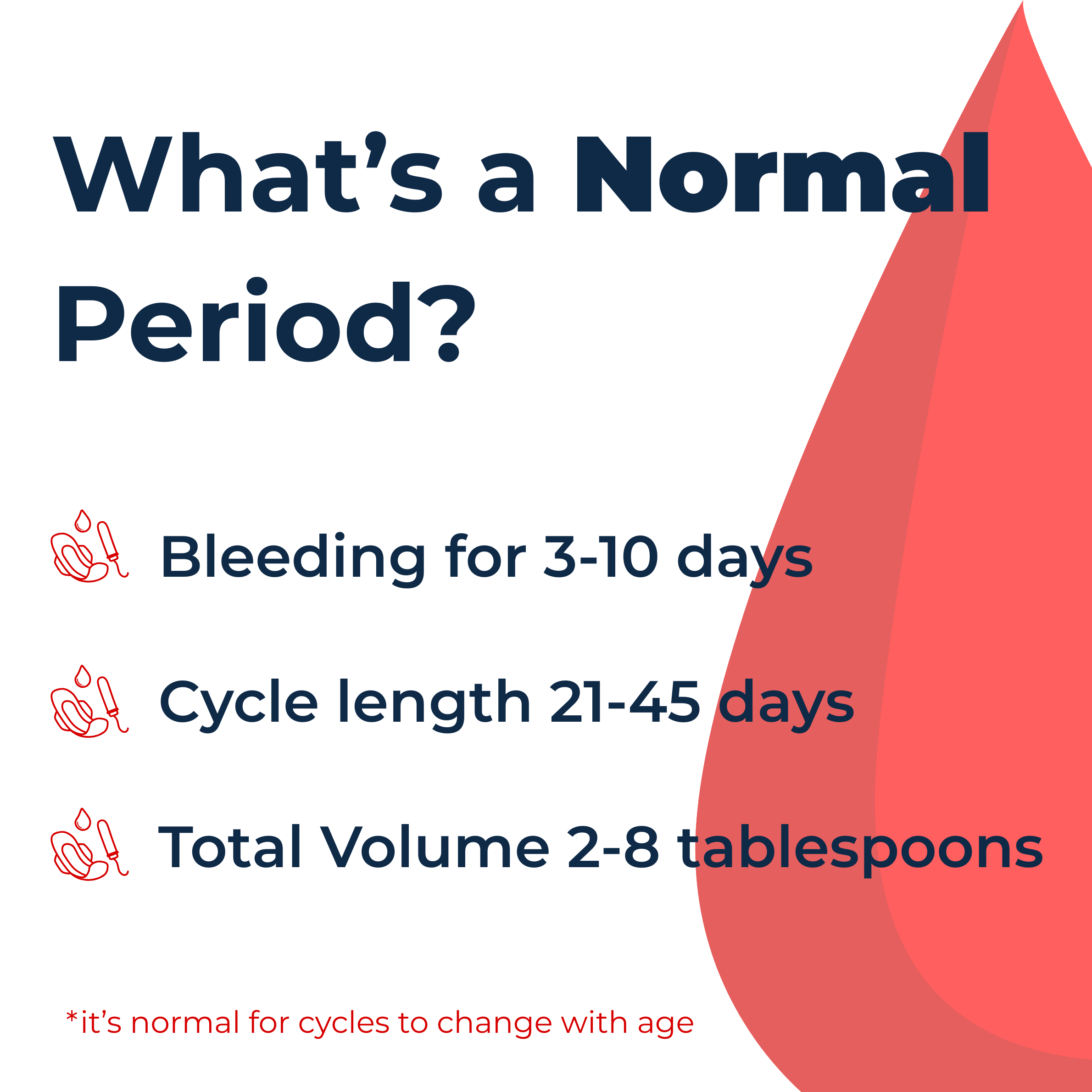
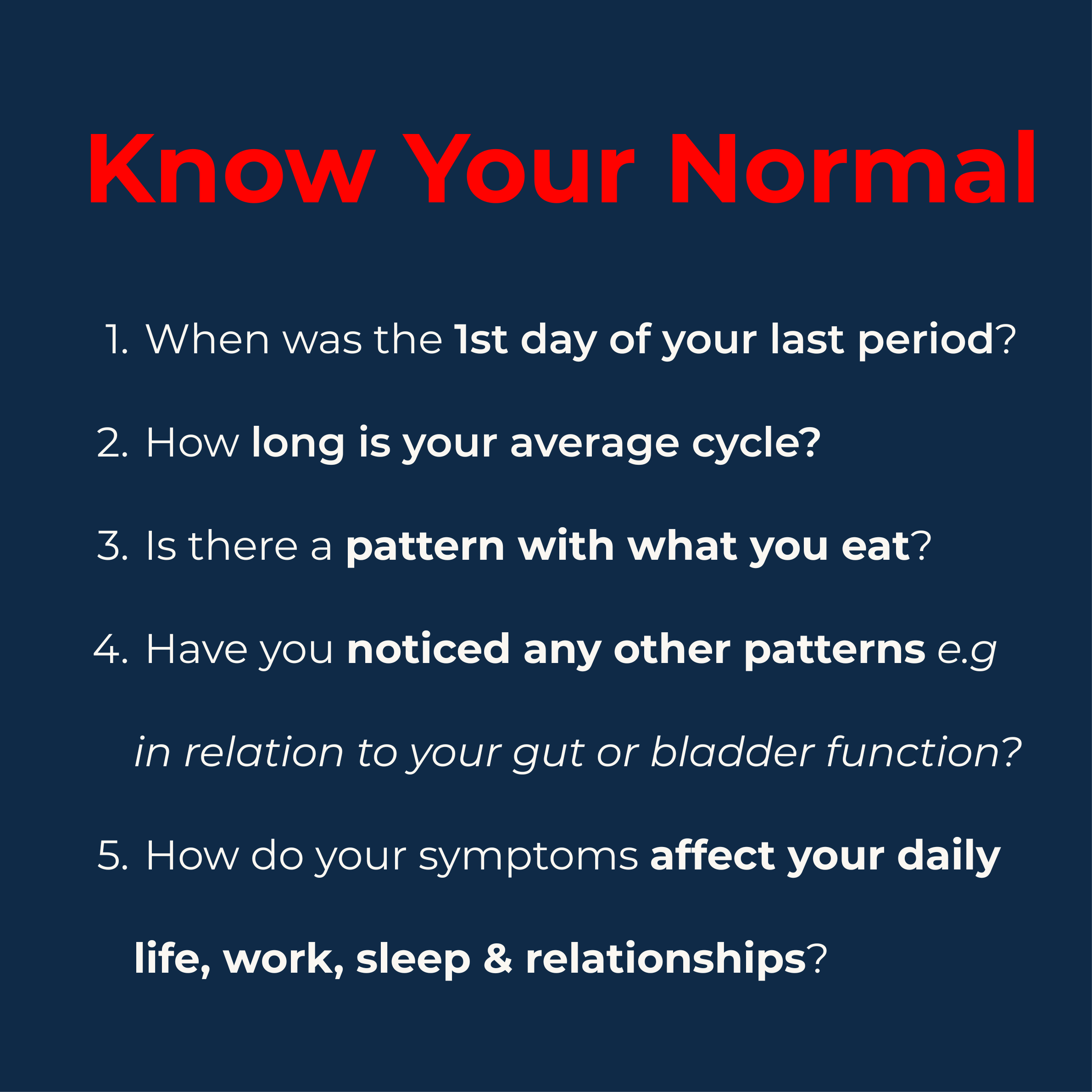
Knowing your normal is, therefore, the number one most important skill you should invest in.
Track Your Symptoms
Use Your B.R.A.I.N to Make Shared Decisions
Think B-R-A-I-N!
This is my favourite prompt to enable shared decision-making. Ask( and answer) these questions:
What are the Benefits of this option?
What are the Risks of this option?
What are the Alternatives?
What’s my Intuition( gut feeling)?
What is likely to happen if I did Nothing?
Your Toolkit for a Great Gynaecology Visit
Here’s how you can walk into your next appointment feeling confident, drawing from my practice and resources from FiveXmore:
Come Prepared: You don’t need to shave or have matching socks- but bring a diary tracking your symptoms over a 4-8weeks.
Share the impact: Talk about how your symptoms affect your daily activities, sleep & relationships
Speak up: Ask about all your options. Think B.R.A.I.N to get the full picture—risks, benefits, and alternatives.
Bring a buddy: A friend or family member can jot down notes or back you up if you’re nervous.
Get a second opinion: It’s your right if something doesn’t feel settled.
Trust your gut: If something’s off, say so. Your instincts matter.
Do your homework: Check trusted sites like NHS.uk or RCOG Patient Information.
Write it down: Keep a notebook for your questions and the answers we share.
The Bigger Picture: Fixing a Stressed System
I won’t sugarcoat it—healthcare providers are human too, and we’re up against a lot: packed schedules, outdated tech, and burnout that’s all too real. The Reimagining study found that low morale and a lack of communication training hold us back from listening as well as we’d like.
But there’s hope.
Policymakers, imagine funding training that helps doctors like me better understand women’s unique needs, like addressing racial disparities in maternal care.
Academic friends, let’s study care models that center lived experience.
Corporations, let’s team up on tech that frees up time for real conversations.
Learning from communities is the best way to make women’s healthcare more accessible
Having worked across diverse settings—from clinics in Edinburgh to community health initiatives in Kyanzanga, Uganda—I’ve witnessed the power of partnership and shared decision making: when clinicians and patients collaborate as equals, outcomes improve, trust grows, and care becomes truly personalised.
Let’s Keep the Conversation Going
Drop a comment, share this post, or shoot me an email at contact@drisiomaokolo.com. Let’s make women’s healthcare a place where everyone feels heard.
👉🏽 Sign Up for My Women’s Newsletter
For more topics like this and a FREE roadmap of essential Female Health Checks