Black Maternal Health in Scotland: the NAUWU Report
Introduction: The Hidden Crisis in Scottish Maternity Care
She was 38 weeks pregnant, excited, and terrified
Let’s call her Amara. A Black mother in Edinburgh who walked into the labour ward believing she’d be heard. Instead, her pain was dismissed as “anxiety.” Her concerns about bleeding? Brushed off as “normal for African women.” Hours later, she lost her baby.
This is not an isolated tragedy. Black women in Scotland are 4 times more likely to die in pregnancy or childbirth than white women; they are more likely to experience a ‘near miss’ adverse outcome and disrespectful, discriminatory care in pregnancy, birth and beyond—a statistic that hasn’t budged in over a decade.
But now, there’s a blueprint for change.
I’m proud to share the NAUWU Maternity Report—Nothing About Us Without Us—published by KWISA (Women of African Descent in Scotland) in partnership with NHS Lothian Maternity Voices Partnership. This isn’t just research.
It’s a movement—built on lived experiences, evidence, and unapologetic demands for equity.
NAUWU( Nothing About Us Without Us) is an initiative designed to amplify the voices of and advocate for Black women navigating the maternity care system in Scotland.
This report, a product of tireless research and heartfelt storytelling, marks a critical milestone in addressing disparities in maternal health outcomes for Black women in Scotland
It goes beyond describing the problem to offering a roadmap for change that includes improved education, enhanced support, and responsive healthcare systems that track and eliminate ethnic minority maternity disparity
What the NAUWU Report Reveals: Stories and Stats
The report doesn’t just describe the problem—it names it.
Black mothers we spoke with reported feeling ignored or dismissed during their pregnancy and birth. Cultural misunderstandings, racial bias, and lack of continuity of care were recurring themes. Women reported that staff were slow to respond to their pain; staff did not know how to recognise medical conditions in darker skin, e.g. anaemia and jaundice. Staff
Voices from Black Mothers
The Numbers Don’t Lie
Other reports and studies highlight:
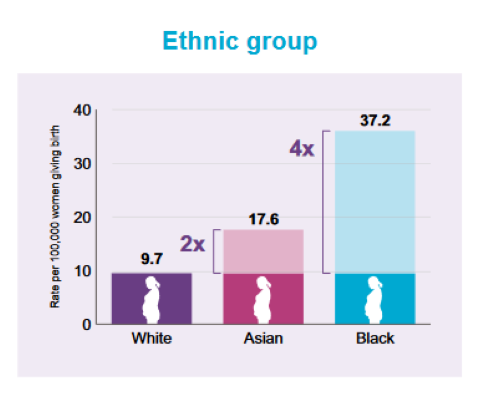
4x higher maternal mortality risk for Black women vs. white women in the UK ( UK MBRRACE)
62% of African/Caribbean women felt their cultural needs were not met ( AMMA Birthing Companions Report)
3 in 5 reported microaggressions from healthcare staff ( FiveXMore Black Maternal Experience Report)
MBRRACE Report 2021- Comparing Maternal Mortality by ethnicity in the UK
These aren’t just numbers—they’re lives, families, futures.
The Road to Equity: Actionable Recommendations
The NAUWU Report doesn’t stop at diagnosis. It prescribes real, scalable solutions:
Mandatory anti-bias training for all maternity staff, with annual refreshers
Culturally responsive care plans co-designed with African and Caribbean community leaders
Ethnicity data tracking in all NHS maternity units to monitor and eliminate disparities
Dedicated Black maternity advocates in every health board
Community birth companions trained in trauma-informed, culturally safe support
Policy Wins: Collaborating with NHS Lothian. As a consultant OBGYN and advocate, I’ve seen what happens when systems listen. NHS Lothian’s partnership with KWISA is already piloting ethnicity-coded feedback loops—a model that should go national.
Why This Matters: Celebrating Resilience and Calling for Change
“We believe that maternity care should empower every woman, embracing her unique needs, culture, and experiences. This report is more than just a call to action—it’s a blueprint for collaboration, education, and policy reform.”
This report isn’t just about survival—it’s about thriving.
It celebrates the resilience of Black mothers who birth, heal, and lead despite the odds. It’s also a reminder: Equity isn’t a privilege. It’s a right.
Too often, the voices of African and Caribbean women are overlooked in the broader maternity care narrative.
Through first-hand accounts, evidence-based analysis, and actionable recommendations, this report shines a spotlight on the systemic barriers and biases that perpetuate unequal care while celebrating the resilience and agency of Black mothers. The NAUWU Report doesn’t stop at diagnosis.
Join the Movement: Your Next Steps
📥 Download the full NAUWU Maternity Report → Get the Report (Free PDF)
Take action today:
🔗 Share this post with your network—tag a midwife, doctor, or policymaker
💬 Comment below: What’s one change you’d prioritize in maternity care?
✉️ Join my community for monthly updates on women’s health, careers, and equity
Quick Poll: What should NHS Scotland prioritize? 🗳️ Reply with: A) Anti-bias training B) Cultural care plans C) Data tracking
Follow @kwisa_women kwisa.org.uk to stay in the loop.
Together, we’re not just bridging evidence and impact—we’re building a maternity system that works for every woman.
References:
MBRRACE-UK Perinatal Mortality Surveillance Report (2023)
NAUWU Maternity Report, KWISA & NHS Lothian MVP (2025)
Dr. Isioma Okolo is a Consultant Obstetrician & Gynaecologist, Harvard MPH, and founder of initiatives amplifying women’s voices in healthcare.